Researchers at Hospital for Special Surgery (HSS) in New York City are enrolling patients in a study evaluating 3dMD technology to reduce x-ray use and improve therapy for scoliosis patients.
Currently, physicians monitor patients with scoliosis using x-rays over a several-year period. This extensive exposure to radiation can be harmful, particularly as scoliosis primarily affects young people. HSS researchers hope the results of the study will lead to an algorithm to estimate the curvature of the spine without the need for x-rays.
At the heart of the approach is a highly accurate 30 camera whole body 3D surface imaging system manufactured by 3dMD, which is engineered to produce three-dimensional maps of the spine in people with scoliosis, according to a media release from Hospital for Special Surgery.
“You can take that image, flip it upside down, slice it and dice it at any level that you want because it’s a mathematical depiction of the surface of the patient,” said Roger F. Widmann, MD, Chief of the Pediatric Orthopedic Surgery Service at HSS, in the release.
“This technology is essentially producing the world’s most advanced selfie, and the benefit is that there’s nothing dangerous about it,” said Howard J. Hillstrom, PhD, director of the Leon Root, MD Motion Analysis Laboratory at HSS and the principal investigator of the study.
“When you image with this system, you can count the number of hairs on a person’s leg.”
The new study combines two recently available imaging technologies: topographical mapping using 3dMD, a proprietary system of high-resolution cameras, and EOS imaging, a dual plane x-ray machine that determines spinal alignment while significantly reducing exposure to ionizing radiation.
The 3dMD system combines information from 30 high-definition cameras to produce a full map of the torso in under a second. The speed of the process is a significant advantage over conventional imaging, according to Hillstrom, who noted that up to 10% to 20% of torso x-rays must be redone because inadvertent movements during the scans distort the picture.
“3dMD is immune to that,” he comments.
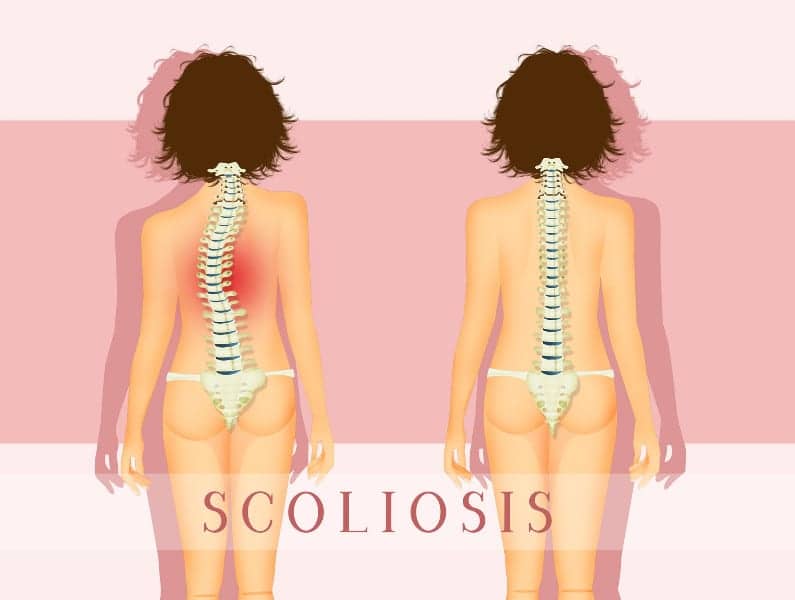
Scoliosis typically is detected when children are in elementary school, during routine screening at school or at their pediatrician’s office. If scoliosis is suspected, clinicians will try to determine the extent of the curvature — mild, moderate or severe — using x-rays. Although mild and moderate cases can improve with physical therapy and bracing, severe cases may require surgery.
“Severe scoliosis starts to affect the symmetry of the thoracic cavity and might then affect lung function,” Hillstrom shares.
Restoring symmetry is a primary goal of scoliosis surgery, Widmann adds, the release continues. However, symmetry is difficult to determine using x-rays, which don’t necessarily reveal how changes to the skeleton affect the shape of the body.
“One of the most important things to patients and families is appearance,” he comments. “That’s what they see and what the world sees. This technology is showing you the surface, and we hope it will help us align the goals of surgery even more closely with what patients and families want from the procedure.”
Anatomical mapping could improve bracing therapy in the same way, he states.
HSS researchers also will be gathering Patient Reported Outcomes Measures (PROMs), such as mobility, personal appearance, ability to participate in sports and other aspects of daily life, and more.
So far, 30 children have enrolled in the study, which Hillstrom and colleagues hope will ultimately include 2,000 patients over the next 5 years, as well as roughly 500 people with normal spines to serve as comparisons.
“Being able to use this technology to screen patients for scoliosis would be a big improvement over the current method, which uses a carpenter’s level on a patient’s back and has a very high rate of false-positives,” Widmann says.
In other words, many children initially suspected of having scoliosis don’t have the condition — but doctors don’t know that until they take an x-ray.
“You’re taking x-rays on a lot of kids who don’t need them, so we need a very reliable technology that correlates with x-rays so that you can safely decide if you need one or not. We’d love to have a better tool for this,” he adds.
The technology might also prove useful for other orthopedic applications, such as creating better casts for custom orthoses and prostheses or estimating inequality in the length of limbs — a problem that can lead to issues with gait, back pain, and other complications.
Portions of the data collected from 3dMD will also be a part of a 3-year competitive research grant that was just awarded to HSS from the Cotrel Foundation entitled, “Use of Surface Topography for Screening and Outcome Evaluation of Adolescent Idiopathic Scoliosis.”
Widmann serves as the principal investigator and Hillstrom as a co-investigator along with a team of pediatric orthopedic surgeons, scientists, engineers, radiologists, pediatric sports medicine specialists, physical therapists, prosthetists/orthotists, pediatricians, and trainees, per the release.
[Source(s): Hospital for Special Surgery, PR Newswire]