A 5-year award from Patient-Centered Outcomes Research Institute (PCORI) is intended to fund a statewide study, designed to benefit stroke patients across North Carolina by helping determine whether longer-term, post-stroke care improves their daily function. PCORI is an independent, nonprofit organization authorized by Congress in 2010. Its mission centers on funding research that will provide patients, their caregivers, and clinicians with the evidence-based information needed to make better-informed healthcare decisions.
A Wake Forest Baptist Medical Center news release reports that a secondary goal of the $14 million award is to measure and reduce the degree of caregiver stress.
The award funds a statewide study led by Pamela W. Duncan, PT, PhD, principal investigator, professor of neurology and senior policy advisor for innovations and transitional outcomes, Wake Forest Baptist Medical Center, co-investigators Cheryl D. Bushnell, MD, director of the Wake Forest Baptist Stroke Center, and Wayne D. Rosamond, PhD, professor of epidemiology, Gillings School of Global Public Health, The University of North Carolina at Chapel Hill. A total of 51 hospitals are also joining in the statewide study. They are part of the North Carolina Stroke Collaborative registry, a partnership between the NC Division of Public Health and UNC-Gillings. Additional collaborators include faculty from Eastern Carolina University School of Medicine Center for Health Disparities and the Duke University School of Nursing.
According to the release, the 5-year study is known as COMprehensive Post Acute Stroke Services (COMPASS). The study will compare patients who receive existing stroke treatment as they are discharged home, to patients who receive comprehensive stroke services once they return home.
In the release, Duncan points out that stroke patients face a high risk of complications once they leave the hospital.
“They often have physical deficits that make falls a common occurrence and there are cognitive problems that make easy tasks like filling a weekly pill dispenser impossible,” Duncan says.
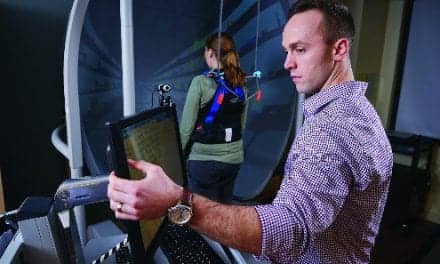
The release states that COMPASS deploys nurse practitioners or physician assistants to coordinate discharge services and assist during the transition from hospital to home. Within 7 to 14 days of discharge, these providers see the stroke patient at their home or in a clinic and, by working with the patient’s caregiver, develop an individualized care plan for each patient. The release notes that a trained community coordinator also works with local organizations to ensure that recovering patients and caregivers have the services and support they require. Regular contact is maintained with the patient and caregiver after discharge for at least 90 days.
COMPASS’ comprehensive components are based upon feedback from stroke survivors who shared their experiences and ideas for improved post-discharge stroke care with study investigators.
The release reports that during the two-phase study, adult patients admitted to a NC Stroke Care Collaborative hospital, diagnosed with stroke and discharged directly from acute care at the hospital to the home will be eligible to enroll. In Phase I, COMPASS and usual care will be compared. Half of the participating hospitals will be randomly assigned to provide COMPASS to all stroke patients at discharge, while the remaining half will provide usual care.
During Phase II of the study, the usual care hospitals will provide COMPASS, while the Phase 1 hospitals will continue to provide comprehensive post-care services. The release says at least 9,000 patients are expected to be reached through this study, which is slated to begin in 2016.
Source: Wake Forest Baptist Medical Center