Stroke affects 800,000 Americans annually,1 the majority of whom go on to live with long-term disability and limited community participation due to impaired ability to walk, stand, and perform transfers. Rehabilitation in the outpatient setting has been shown to reduce disability, promote independence with activities of daily living (ADL) and community mobility, and prevent re-hospitalization. Stroke survivors present with a wide range of deficits spanning multiple physiologic systems, and individualized patient-centered care is essential for optimizing rehabilitation success.
Person-centeredness, defined in health care as “meeting a person’s needs, values or preferences … and fully involving persons’ perspectives into care,” is widely regarded as a standard of care across rehabilitation systems. Patient-centered care looks at the individual as an expert whose voice should be at the center of all decision-making. Care is not delivered to the patient, but rather with or for the patient.2 In the outpatient setting, patient-centered care for individuals post-stroke is prioritized and implemented through establishing an individualized and cohesive multi-disciplinary team, utilizing evidence-based outcome measures that highlight limitations in body structure and function, activity, and participation levels, and selecting low-tech and high-tech interventions that are targeted and salient to patient goals.
Multi-disciplinary Team
At Good Shepherd Rehabilitation Network’s outpatient Health & Technology Center, Allentown, Pa, members of the stroke multi-disciplinary team include on-site physiatrists, neuro-psychologists, case managers, and a neuro optometrist. This team works closely with a vision rehabilitation team, as well as physical therapists, occupational therapists, and speech therapists. To optimize communication among team members, panel meetings occur weekly between all disciplines. Meetings with patients, their families, and caregivers are scheduled with case management and members of the interdisciplinary team to help patients and families develop an individualized care plan based around the patient’s desires, needs, and goals. Close collaboration often occurs with local bracing and orthotics vendors, as well as our seating and mobility clinic to meet patients’ individual functional needs.
From a physical therapy standpoint, it is essential during the initial evaluation process to get a comprehensive sense of the individual and his or her support system, as well as the functional capabilities required for performance of ADLs and negotiation of his or her home and community. The initial driver of this process is a thorough subjective history. From there, a selection of reliable, valid outcome measures that have good clinical utility among neurologic populations serve to tease out specific body structure and function, activity, and participation-level limitations on functional mobility that are meaningful to the patient.
Standardized Outcome Measurement
The Academy of Neurologic Physical Therapy (ANPT) published a clinical practice guideline in 2018 outlining a core set of outcome measures for adults with neurologic conditions, specifically covering constructs of balance, walking speed, walking endurance/distance and transfer ability.3 These measures include: 6-minute walk test, 10-meter walk test, Berg Balance scale, Functional Gait Assessment, Activities Specific Balance Confidence Scale, and 5 Times Sit to Stand. Utilization of this standardized and evidence-based set of outcome measures enables clinicians to systematically track patient progress and re-examine effectiveness of selected treatments.
In addition to this core set of outcome measures, the ANPT has developed highly recommended stroke-specific outcome measures to be utilized in the outpatient rehabilitation setting. The Stroke Impact Scale is a self-report measure that assesses quality of life and health status under the domains of strength, hand function, ADLs, mobility, communication, emotion, memory, and participation. Repeated administration of this questionnaire provides therapists with insight into patients’ evolving perceptions of their deficits and can be a useful aid in guiding meaningful goal-setting. The Stroke Rehabilitation Assessment of Movement is an objective measure used to evaluate motor function after stroke in the context of upper- and lower-limb movements and basic mobility activities. It can be a useful tool in highlighting coordination, range of motion, and functional mobility impairment that limit meaningful household and community activities like bed mobility, transfers, walking, and stair negotiation to drive individualized treatment approaches. A comprehensive list of recommended outcome measures at each level of care post-stroke can be found on the ANPT website.
Technology Addresses Individual Deficits
In addition to utilizing evidence-based standardized outcome measures, Good Shepherd Rehabilitation Network has a variety of technologies that aid in assessment and development of interventions for postural, gait, and balance deficits. In combination with lower-profile methods, these are a foundation to develop comprehensive plans of care based on patients’ individual deficits and needs.
Falls are particularly common after stroke, occurring in up to 73% of patients within the first 6 months after injury.4 Both falling and fear of falling can be significant limiting factors to activity and participation. Balance disturbances have a variety of origins in the hemiparetic patient, including decreased strength and range of motion, abnormal muscle tone, impaired motor control, impaired sensory organization, and visual deficits. Root causes of balance impairments and resulting compensatory strategies are highly variable among patients and can be difficult to tease out with utilization of observational standardized outcomes only.
Computerized Dynamic Posturography uses Sensory Organization Testing to systematically deprive visual, vestibular, and somatosensory inputs to determine how much a patient relies on each system and how well the systems are integrating to maintain balance.4 The patient stands on a force plate, and kinetic data shows postural reactions during removal of different sensory inputs. Results of Sensory Organization Testing are compared to age-matched norms and used to develop interventions that address specific components of overall balance control to improve postural stability, reduce risk of falls, and enhance patient confidence with standing, walking, and negotiating elevations.
Several technologies are available that can provide this type of testing to help therapists zero in on balance disorders, including the Bertec CDP balance system from Columbus, Ohio-headquartered Bertec. The system can conduct tests that assess how a patient responds to stimuli while standing on a surface that is firm or moving, with and without visual cues. As an example, during the motor control test, when the floor of the device suddenly moves, the device’s computer measures the time it takes a patient to right himself. Data about the patient’s performance in comparison to age-based norms is then fed back instantly to the therapist.
The Biodex Balance System SD from Biodex, Shirley, NY, is another technology that is designed to help improve an individual’s balance and agility in addition to a number of other pathologies. The SD is built to help assess neuromuscular control by quantifying a person’s ability to maintain dynamic bilateral and unilateral postural stability on a surface that is static or unstable. The Balance Master family of technologies from NeuroCom, Pleasanton, Calif, are also built to provide visual feedback using a stable or unstable support with a visual environment that can be stable or dynamic. These systems, too, provide objective data to address the issues that underlie an individual’s functional limitations.
Stroke survivors often exhibit altered kinematic and muscle-activation patterns secondary to weakness and abnormal muscle tone, manifesting in profound gait deficits. Common deficits include decreased velocity and cadence and increased double-limb support time, as well as increased swing phase and shorter stance phase of the hemiparetic limb as compared to the contralateral limb.5 This results in increased energy expenditure and risk of falling, thereby limiting community participation and involvement. For these reasons, assessment of gait kinematics is essential to promote optimal gait recovery.
Software Analyzes Gait Deficits
Good Shepherd Rehabilitation Network utilizes Simi Motion 2D/3D gait and functional movement analysis software to supplement observational analysis and objectively assess hemiparetic gait. Movement data recordings are obtained with use of synchronized cameras, force plates, and joint markers. The software calculates joint angle, velocity, and positional changes that contribute to gait deficits. Visual representation of this data can be a meaningful educational tool for gait retraining, promoting enhanced collaboration between the patient and therapist as well as knowledge-of-results feedback to enhance motor learning. This software can assist with collaborative decision-making regarding appropriate assistive devices or orthotics to optimize safety and independence with walking.
Other technologies that can help therapists evaluate gait include the GAITRite systems from CIR Systems, Franklin, NJ, which are designed to measure temporal spatial parameters of gait by using an electronic walkway connected to a computer. Also available is the Zeno Walkway from ProtoKinetics, Havertown, Pa, a gait analysis platform that uses PKMAS software to collect and analyze temporal, spatial, and pressure data in addition to symmetry of propulsion. Another device, the BodiTrak 2 from Vista Medical, Winnipeg, MB, Canada, is a balance sensor mat that is flexible, portable, and designed to be used on a variety of surfaces including a step, balance board, air bladder or foam, or flat on the floor.
Robotic Exoskeletons
Many gait impairments observed post-stroke manifest as a result of unilateral hemiparesis, sensory and proprioceptive deficits, and visuospatial deficits. Wearable robotic exoskeletons enable individuals to walk overground with full weight bearing and a reciprocal gait pattern in order to relearn normalized mechanics with intensive step dosage over ground.6 EksoGT robotic exoskeletons from Ekso Bionics, Richmond, Calif, are utilized at Good Shepherd to promote gait symmetry and upright posture, and facilitate optimal weight shifting while limiting common compensatory strategies. The software is customizable to allow for varying swing limb assist and stance control in each lower extremity for maximal active contribution from the patient, with the goal of promoting long-term carryover for improved walking mechanics, safety and efficiency in household, and community ambulation.
Self-Corrections for Enhanced Motor Learning
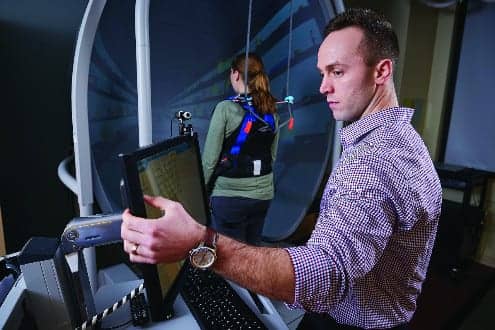
Effective functional retraining after stroke can be limited by safety concerns and increased required levels of assistance. Good Shepherd utilizes the ZeroG Gait & Balance System from Aretech LLC, Ashburn, Va, to provide a safe and controlled environment where patients can work toward completing household mobility tasks like transfers, walking and elevation training in the context of their individual goals. The robotic dynamic bodyweight support via overhead harness, coupled with advanced falls protection technology, allows patients to be more independent and provides them with the opportunity to make self-corrections for enhanced motor learning. The system also records metrics like total distance walked, total training minutes, and number of falls prevented to assist with tracking patient progress and can be utilized as an educational tool.
The physical therapy marketplace offers several additional types of technologies that leverage robotic technology to address gait issues. One such technology is the Lokomat from Hocoma, Norwell, Mass. This device uses an adjustable robotic gait orthoses and dynamic body weight support over a treadmill to facilitate highly repetitive gait training, which may be a benefit especially to individuals who are severely impaired. The Lokomat is designed to be useful in supporting treadmill training in the treatment of individuals affected by walking disabilities caused by neurological, muscular, or bone-related disorders.
In addition to utilizing assessment and intervention strategies that revolve around patients’ individual desires, needs, and lifestyle choices, Good Shepherd Rehabilitation Network is committed to providing preventative education and screening through outreach programs as a means to promote health literacy and wellness in our community. Good Shepherd also facilitates stroke support groups aimed at enhancing quality of life and optimizing advocacy by educating patients and their caregivers and families about up-to-date advances in rehabilitation. PTP
Kelley Limbauan, PT, DPT, is a neurologic resident at Good Shepherd Rehabilitation Network, Allentown, Pa. For more information, contact [email protected].
References
1. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2017;48(2). https://www.doi.org/10.1161/str.0000000000000120.
2. Jesus TS, Bright F, Kayes N, Cott CA. Person-centred rehabilitation: what exactly does it mean? Protocol for a scoping review with thematic analysis towards framing the concept and practice of person-centered rehabilitation. BMJ Open. 2016;6(7). https://www.doi.org/10.1136/bmjopen-2016-011959.
3. Moore JL, Potter K, Blankshain K, Kaplan SL, O’dwyer LC, Sullivan JE. A core set of outcome measures for adults with neurologic conditions undergoing rehabilitation. J Neurol Phys Ther. 2018:42(3):174-220.
4. Oliveira CB, Medeiros ÍRT, Greters MG, et al. Abnormal sensory integration affects balance control in hemiparetic patients within the first year after stroke. Clinics (Sao Paulo). 2011;66(12):2043-2048. https://www.doi.org/10.1590/s1807-59322011001200008.
5. Ferrarello F, Bianchi VAM, Baccini M, et al. Tools for observational gait analysis in patients with stroke: A systematic review. Phys Ther. 2013;93(12):1673-1685. https://www.doi.org/10.2522/ptj.20120344.
6. Ekso GT Redefines Gait Training, Introducing a New Generation of Ekso. Richmond, California: Ekso Bionics Inc; 2013.
Electronic Walkways 101
By Frank Long, Editorial Director, Physical Therapy Products
Digital technologies such as electronic walkways and related devices are changing the way therapists measure gait. These systems are quickly evolving, so prospective buyers should know the basics about them before making a purchase.
do the homework
According to Michael Rowling, Chief Operating Officer, ProtoKinetics, Havertown, Pa, manufacturer of the ProtoKinetics Zeno Walkway, due diligence is essential to making a smart purchase. That means educating oneself about the available technologies, comparing what they do, and participating in a hands-on demonstration, if possible.
“It’s critical to compare and contrast real-world proof and results, and not just believe the marketing hype from the results you might get in a Google search or a seemingly impressive magazine advertisement,” Rowling says. He emphasizes that data must be robust, and points out that tasks such as capturing and analyzing difficult gaits, or capturing data about turning, are functions that need to be demonstrated.
“That part of the process can help determine whether the technology backs up the marketing messages,” Rowling says.
What’s in a Walkway?
Walkway technologies can vary in detail and appearance but, simply stated, a walkway is an integrated system designed to provide an objective picture of gait, says Karen Toepper, Vice President, Sales, CIR Systems, Franklin, NJ, manufacturer of the GAITRite family of electronic walkways.
“As the patient ambulates across the walkway, a sensor technology measures numerous measures of gait,” Toepper explains. “A walkway is considered one of the most accurate measurement tools and is often used to validate other devices such as wearable sensors,” she adds.
Toepper points out that the importance in detecting a person’s gait issue can play a significant part in the individual’s present and future health, and gather important data to study concerns such as cardiovascular conditions, musculoskeletal problems, neuromuscular disorders, and other conditions.
“Just a few passes across the walkway and data is collected that will help tremendously in determining the issue,” she adds.
Floor-Based Option
The current market of gait analysis technologies includes compact systems that use sensing pads. The pads can be retrofitted to treadmills that use smooth decks or belts, or integrated by manufacturers into their own treadmill designs. The result is a smaller footprint and smaller investment. One such device, the BodiTrak2 from Vista Medical Ltd, Winnipeg, Manitoba, Canada, uses treadmill sensors that are a variation of stand-on-balance mats.
Andrew Frank, Chief Operating Officer, Vista Medical Ltd, explains that the BodiTrak2 sensors can be incorporated into rehab protocols for Parkinson’s disease as well as to treat concussion, and are used in dynamic and static assessment modes.
“Some of the well-known walkway systems can take up lots of space in a clinic, and be costly,” Frank says. “We’ve designed BodiTrak2 as a system that can capture and display how symmetric and stable the walking or running patient is, but do it in a smaller space with more affordable technology.
Frank notes that many of the rehab professionals with whom he speaks agree that full-size walkways have an edge on treadmill-based technologies where intensive research is being conducted. In contrast, however, for the average clinic treating rehab clientele, those types of larger systems take up too much space and are costly, Frank adds.