The field of post-concussive care is actively evolving, as is evidenced by ongoing media presence, emerging medical evidence, and rule changes in sports, to name a few examples. What was a passive “rest is best” treatment approach has evolved into a much more active and engaged recovery process following the initial rest phase. Recent evidence suggests that rest beyond 2 days prolonged symptomatic recovery.1 That being said, understanding individualized treatment approach, symptom thresholds, and concussion clinical profiles is essential to safe and effective treatment in the post-concussive population.
[sidebar float=”right” width=”250″]Product Resources
The following companies offer technologies for vestibular rehabilitation and treatment of dizziness:
Biodex Medical Systems
www.biodex.com
Hoggan Scientific LLC
www.hogganhealth.net
Micromedical by Interacoustics
www.micromedical.com
Natus Medical Inc (NeuroCom)
www.onbalance.com
novel electronics
www.novelusa.com
Perry Dynamics Inc
www.perrydynamics.com[/sidebar]
While determining accurate clinical trajectories may be challenging, it is critical that a multidisciplinary approach to assessment and treatment is utilized. Various specialists are able to assess various physiologic, medical, and mechanical systems to identify impairments associated with the post-concussion sequelae. At Good Shepherd Rehabilitation Network, concussion team members include physiatrists, physical therapists, occupational therapists, vision therapists, speech therapists, neuro psychologists, and a neuro optometrist.
As with varied healthcare practitioners who support the post-concussion team, concussions also can vary in the way symptoms manifest. Among the constellation of physical, cognitive, emotional, and sleep symptoms following a concussion, it is valuable to healthcare practitioners to understand the pathophysiology and body systems affected by a concussion/mild traumatic brain injury. Common symptoms include dizziness, headaches, mood disorders, balance impairments, and/or light sensitivity.
Clinical Profile
This understanding of the various subsystems of concussive care is pivotal to the patient’s prognosis, and this subsystem classification has been proven effective in the literature. Establishing the clinical profile(s) is determined by subject history, clinical objective findings, and exertional tolerance.2 As treatment paradigms are focused on the aforementioned clinical profiles, one challenge of post-concussive care is that it is common for more than one profile to be involved. It is rare that only one clinical profile is present. The context of this article will focus on vestibular rehab in the realm of post-concussion care.
In the vestibular clinical profile, it is common for patients to report dizziness, imbalance, visual motion sensitivity, blurry vision, fogginess, etc. In a study published by Bara Alsalaheen, dizziness is a frequent symptom of concussion and has been reported to occur in 23% to 81% of cases in the first days after injury.3 In the acute phase of a concussion, subjective reports of dizziness are understood to predict protracted recovery. Therefore, early identification of vestibular-related issues can help to speed recovery. There are numerous ways to assess vestibular dysfunction, and the Comprehensive Concussion Program at Good Shepherd Rehabilitation Network utilizes both handheld and technological assessment tools to evaluate and treat subjects that fall within criteria for vestibular-related deficits because of a concussion.
ASSESSMENT AND TREATMENT TECHNOLOGIES
Video Goggles
Though positional vertigo is relatively uncommon in traumatic brain injuries, it is essential to have effective treatment to identify associated positional impairments. Video goggles, when placed over a patient’s eyes, similar to scuba goggles, are used to assess positional vertigo, nystagmus, and identify vestibular hypo-functioning. Video goggles can assist in the therapist’s ability to clearly identify nystagmus present via a subject’s eye through video magnification without visual fixation. In turn, capturing pertinent information about a subject’s eye during position changes can dictate treatment paradigms depending on direction and duration of ocular movement. This phenomenon is consistent in the assessment and treatment of benign paroxysmal positional vertigo (BPPV).
Video goggles also are used in the assessment of peripheral vestibular dysfunction in which a patient’s gaze stability, nystagmus, and ocular movement are evaluated. Through various tests utilizing head and eye movements, therapists are more accurately able to capture information about appropriate vestibular functioning using fixation removed ocular movement in video goggles. Much of vestibular rehabilitation in the post-concussion population is focused on improving one’s gaze stability—the ability to maintain focus on an object when the head is in motion. This function is known to be the vestibular ocular reflex (VOR). The understanding of abnormal test results gathered during handheld and technological testing provides the therapist with distinctive treatment protocols for remediation. Parameters can include duration, speed, and compliance of surface and background interference during training patterns. While the visual and vestibular systems are closely married, the context of this article will not highlight the deficits associated with visual dysfunction following a concussion.
Video goggles are available to the physical therapy market from several sources, including Micromedical Technologies Inc, Chatham, Ill, which manufactures the VisualEyes 505 Binocular video goggles. The VisualEyes 505 can record both eyes with or without vision, and may be used while performing the Dix-Hallpike test to make a Benign Paroxysmal Positional Vertigo (BPPV) diagnosis. The company also offers the VisualEyes 525 Video Nystagmograph as a high speed binocular goggles that can objectively record horizontal and vertical eye movement to test balance and dizziness disorders. Other sources for video goggles include VestibularFirst, which offers the Insight infrared video goggles,
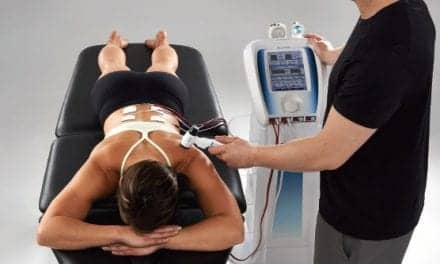
Computerized Posturography
In addition to perceived dizziness and impairments in gaze stability with positional changes and body and head movement, vestibular dysfunction can lead to impairments in balance and postural stability. Good Shepherd Rehabilitation Network utilizes computerized dynamic posturography for postural sway, balance, and sensory organization assessments. Multiple physiologic pathways contribute to one’s balance, including visual, somatosensory, and vestibular inputs. Computerized posturography technology provides immersive virtual stimuli that can assist therapists’ ability to discern impaired pathways and provide a framework for treatment intervention to address these deficiencies.
The use of this highly technological equipment affords the therapist an opportunity to look at the interaction of these three subsystems under a metaphorical microscope. Knowledge of postural sway subsystem impairments allows a therapist to create impairment-based treatment regimens for optimal recovery. In simulated virtual reality environments created within this computerized equipment, therapists are able to fabricate vestibular motion, spatial awareness modules, visual flow scenarios, and biofeedback programs to remediate balance impairments. Treatment to remediate balance impairments, similar to gaze stability, is graded by increased complexity of stimuli, speed, motion, and visual closure. Computerized balance systems for the PT market are provided by several manufacturers, including the Balance System SD from Shirley, NY-headquartered Biodex. The system uses a pressure plate on an unstable surface to test for balance and stability. The system can also be used as a training device for proprioception, stabilization, range of motion, and weight shift exercises.
Though Good Shepherd Rehabilitation Network utilizes advanced technology to aid in vestibular dysfunction identification, handheld tools such as letter charts, object tracking, and visual fixation during head/body movement must be utilized to corroborate findings.
In a systematic review published by Kathryn Schneider, vestibular rehabilitation has demonstrated positive symptomatic and functional improvements in patients who have suffered mild traumatic brain injuries of all types.4
Video Motion Analysis
As vestibular dysfunction can lead to movement and balance impairment, evidence suggests that concussion history is correlated to musculoskeletal injuries.5 Considering this, Good Shepherd Rehabilitation Network utilizes video motion analysis software to assess biomechanic movement impairments during functional movement patterns. Understanding that the vestibular system contributes to balance, biomechanical analysis of movement using high-definition two- and three-dimensional video feedback provides an efficient tool to analyze impairments and provide treatment to reduce the risk for future musculoskeletal or concussion injuries.
It all checks out
Prior to re-integration into work, academic, sport, or recreational settings, Good Shepherd Rehabilitation Network prides itself on a concussion “check-out process.” During this process, patients are put through testing of all concussive clinical profiles to ensure proper physiologic subsystem functioning. Using the aforementioned technologies and assessment/treatment tools, therapists are able to confidently re-immerse their patients back into their premorbid level of functioning.
Stephen Vandenberg, PT, DPT, ITPT, is a staff physical therapist at Good Shepherd Rehabilitation Network, Allentown, Pa. For more information, contact [email protected].
References
1. Haider MN, Leddy JJ, Pavlesen S, et al. A systematic review of criteria used to define recovery from sport-related concussion in youth athletes. Br J Sports Med. 2018;52(18):1179-1190.
2. Ellis MJ, Leddy JJ, Willer B. Physiological, vestibulo-ocular and cervicogenic post-concussion disorders: an evidence-based classification system with directions for treatment. Brain Inj. 2015;29(2):238-248.
3. Alsalaheen BA, Mucha A, Morris LO, et al. Vestibular rehabilitation for dizziness and balance disorders after concussion. J Neurol Phys Ther. 2010;34(2):87-93.
4. Schneider KJ, Leddy JJ, Guskiewicz KM, et al. Rest and treatment/rehabilitation following sport-related concussion: a systematic review. Br J Sports Med. 2017;51(12):930-934.
5. Pietrosimone B, Golightly YM, Mihalik JP, Guskiewicz KM. Concussion frequency associates with musculoskeletal injury in retired NFL players. Med Sci Sport Exerc. 2015; Available at: http://www.trazer.com/pdfs/support/concussion-frequency-associates-with.pdf. Accessed February 6, 2019.